Howard County schools spent $8M on GLP-1 weight-loss drugs — then pulled the plug
The Howard County Public School System learned to the tune of $8.2 million in less than a year just how popular the newest weight-loss drugs had become with its teachers and other employees.
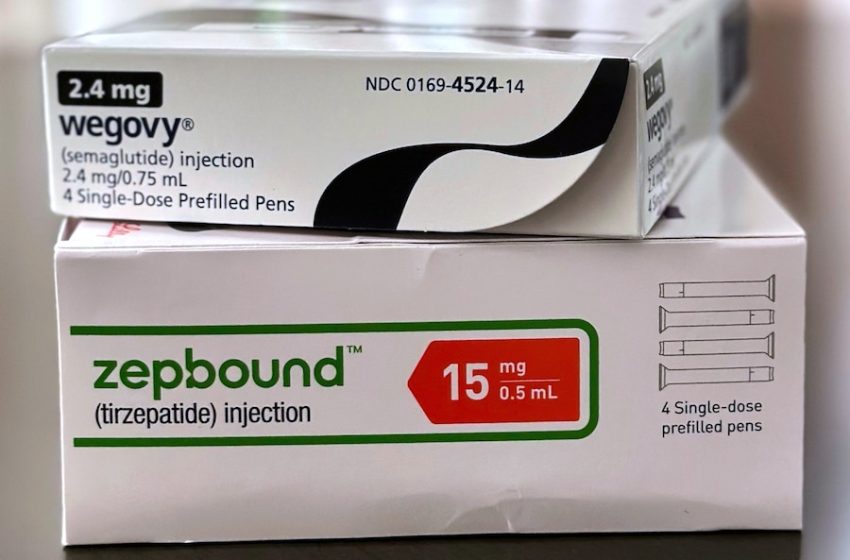
So many of the system’s employees have been prescribed medications known by the brand names Wegovy, Mounjaro and Ozempic that the system can no longer afford to pay for them. It is ending most coverage of the drugs next month, curbing costs that have skyrocketed 600% in two years.
The school system is among a growing list of employers scaling back coverage of the drugs after they surged in popularity in recent years. Originally developed to treat diabetes, the medications are frequently prescribed for people with obesity and other conditions that can improve with weight loss. As the costs rise for health insurance plans, more are putting patients on the hook to pay.
Starting March 31, the Howard County school system will limit coverage of the medications, also called GLP-1 agonists, to people with diabetes. The move will prevent health insurance premiums from rising nearly 20% for everyone, school system officials said.
In 2023, the school system spent $1.6 million in claims for 263 employees who were prescribed GLP-1s for weight loss. Nine months into 2025, the cost had jumped by $6.6 million for 1,144 individual prescriptions. That number represents nearly 10% of the roughly 11,000 employees and retirees on the school system’s heath plans.
One of them is a special education teacher who was prescribed Wegovy nearly two years ago to lower her blood sugar levels. The teacher spoke on condition of anonymity to keep her health condition private from coworkers.
She said she tried working with a nutritionist and exercising but her blood sugar wouldn’t budge. It began creeping into prediabetic territory, putting her at high risk to develop Type 2 diabetes, a chronic condition that can have serious complications, including heart disease, kidney damage and nerve damage.
Within three months of starting Wegovy, her blood sugar levels had lowered.
Now, nearly two years later, her levels are out of the prediabetic range and she’s lost nearly 30 pounds. She said she has more energy and lower cholesterol. She doesn’t want to stop taking Wegovy.
“I’m really on it for other issues going on with my body, and I’m healthy now,” she said. “It’s not just there for weight loss.”
GLP-1s can be a preventive medication for patients with obesity, said Dr. Jung-Im Shin, an associate professor at the Johns Hopkins Bloomberg School of Public Health.
“If we intervene before they [patients] develop diabetes, it will help future health outcomes,” Shin said.
But, Shin said, if insurance stops covering the medications for nondiabetic patients, they may delay treatments for obesity and develop Type 2 diabetes after all.
“If a blanket policy is only applied to the diabetes patient, a lot of people who potentially benefit from these medications will lose the opportunity. I think that’s a huge concern,” Shin said.
Currently, the special education teacher spends $10 a month on her prescription. That cost could jump to several hundred dollars when the school system health plan stops covering it. She said she’s talking to her doctor about her options.
The school system’s benefits advisory committee — made up of school board members, employees and retirees — recommended the health plan stop the coverage for employees who take the medication for weight loss because of the escalating cost.
CVS Caremark, which manages prescription benefits for the school system, did not return a request for comment.
Lynne Cotter, a senior health policy research manager for KFF, said by drug standards the cost of GLP-1s “is not terribly expensive” but the expenses add up once companies consider how many employees are taking the medications.
“The price of these drugs is completely in flux,” Cotter said.
Although patients can find lower prices directly through drug companies, employers don’t always score the deals, oftentimes paying a higher price for the same medication, Cotter said.
A KFF 2025 employer health benefits survey found that, while there was “a notable increase” in companies with more than 5,000 employees covering GLP-1 medications for weight loss, many employers echoed concerns about the cost and number of prescriptions, leading them to consider scaling back.
“The story on GLP-1s is not yet written,” Cotter said. “And every year companies will have to grapple with how much they are spending, how much demand there is for it, how important it is to their workforce and also what the price is.”
First Appeared on
Source link






