Monday marks a full year of continuous measles transmission in Canada, a milestone that’s poised to set the country back decades on a global health commitment. Ongoing transmission in the United States puts it among a group of countries that also face scrutiny from international leaders and are at risk of a similar fate.
All of the World Health Organization’s regions have committed to eliminate measles by 2030, defined by the absence of local virus transmission for any period longer than 12 months. Canada achieved this goal in 1998, but falling vaccination rates set the stage for cases to grow into a massive — and ongoing — outbreak, putting the country and region at risk of losing elimination status.
In early November, the Pan American Health Organization, a regional WHO office, will convene an annual meeting of its Measles and Rubella Elimination Regional Monitoring and Re-Verification Commission to formally determine the status of measles elimination across the region.
“A country is no longer considered to be measles free if the virus returns and transmission is sustained continuously for more than a year,” WHO said in a statement. “There are no formal consequences of losing measles elimination status, however having measles again as an endemic disease will have a profound negative impact on communities, including preventable deaths among some of the most vulnerable populations.”
Countries that lose elimination status will be asked to submit a corrective action plan, which may include efforts focused on intensified vaccination activities, strengthened surveillance and rapid outbreak response.
In 2016, the Americas became the first and only region to effectively eliminate measles by ending local spread. Venezuela and Brazil have both lost elimination status since then, only recently becoming reverified after years of “extensive vaccination, surveillance, and rapid response efforts,” PAHO said. The region as a whole regained elimination status last year, but it is under threat again.
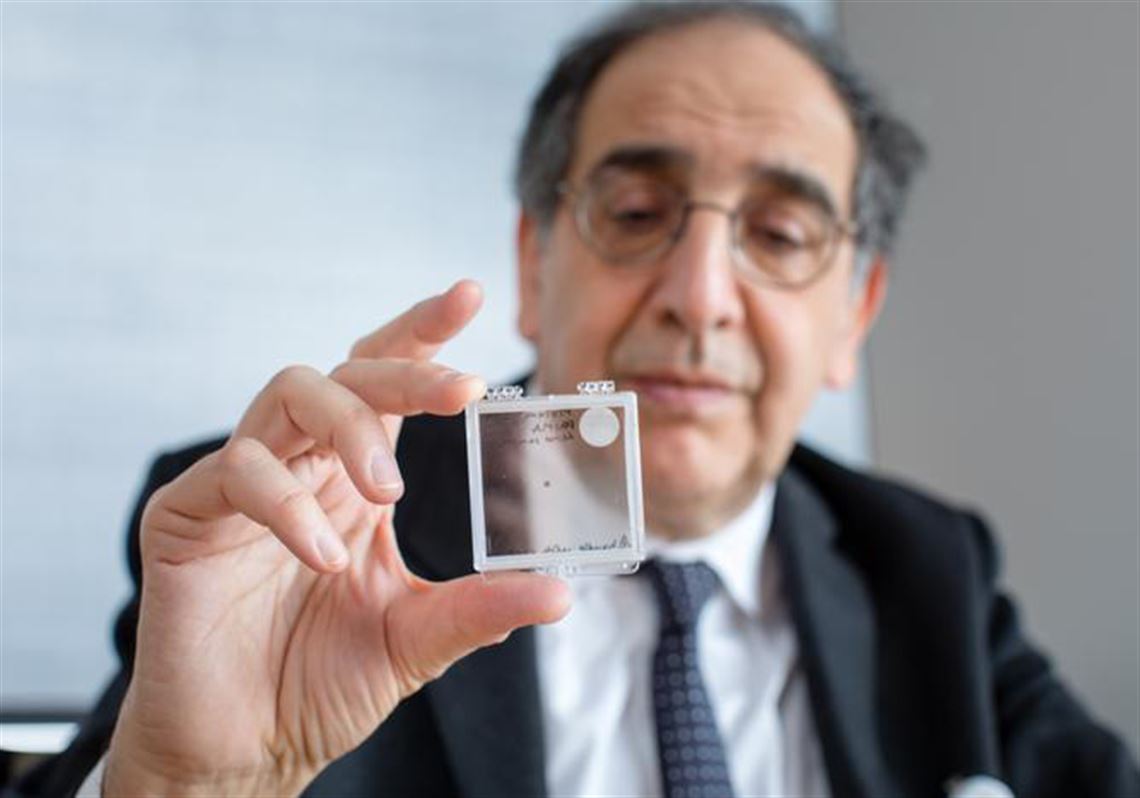
International travel was the initial source of the outbreak that started in Canada in October 2024, according to the Public Health Agency of Canada. But the country has now had thousands of cases across 10 jurisdictions, including hundreds of hospitalizations and two deaths in infants who were born prematurely with infections they contracted before birth.
Canada has tallied more than 5,000 cases this year, more than twice as many as the country has recorded in the past 25 years combined. All but 157 cases have been associated with the outbreak, and about 90% of all cases have been among people who are unvaccinated.
“Immunization coverage across the Region is insufficient to stop outbreaks from occurring, and also hides pockets within countries that have even lower coverage. The Region needs to sustain high coverage, quality surveillance and rapid response at all times,” WHO said.
Canadian leaders are “more consistent” in their support of vaccination than American leaders, said Dr. Dawn Bowdish, an immunologist and professor in the Department of Medicine at McMaster University in Ontario. National surveys suggest that the vast majority of parents still support childhood vaccinations, she said, but health care disruptions from the Covid-19 pandemic, disinformation and misinformation and liberal exemption rules in some provinces have created vulnerabilities.
The potential to lose elimination status “highlights the severity of the measles outbreak,” Bowdish said. “If you look at the other countries that also have circulating measles, you see that they are countries without strong public health like Canada and they are countries that have been torn apart by war or civil unrest. It is an eye-opener about how you need to have constant vigilance and consistent support for public health in order to fight infectious disease.”
Canada’s national health agency says it is in regular communication with the Pan American Health Organization about the progress of the outbreak and efforts to contain it. The outbreak has slowed in recent weeks, the agency says, but there were still 30 new cases reported in the latest week of data available.
And Canada isn’t the only country posing a risk to the region. Six others — including the US and Mexico — have active measles transmission situations that will be discussed at the PAHO commission meeting. President Donald Trump issued an executive order in January to withdraw the US from WHO, but PAHO says that it expects US officials – both from the CDC and the National Sustainability Commission – to attend the commission meeting on measles elimination next month.
In August, local health officials declared that an outbreak centered in West Texas — one of the largest and deadliest in decades — had ended. The outbreak caused 762 cases over the course of about seven months, according to data from the state health department; neighboring New Mexico also reported 100 cases this year associated with the outbreak. Three people died: two children in Texas and one adult in New Mexico, all unvaccinated.
But measles counts continue to grow in the US, and ongoing outbreaks in multiple states — including one on the border of Arizona and Utah and one in South Carolina — are being investigated for possible connections to the Texas outbreak. If links are confirmed and cases continue to spread into January, the US will have also lost its claim to the measles elimination status that it earned in 2000.
The US Centers for Disease Control and Prevention considers the elimination of measles an historic achievement, credited to a “highly effective vaccination program” in the US and better measles control across the Americas region.
But coverage with the measles-mumps-rubella (MMR) vaccine has been declining in the US and Canada for years, with notable dips after the Covid-19 pandemic.
Last school year marked the fifth year in a row that MMR coverage among kindergartners in the US had been below the federal target of 95%, a benchmark needed to prevent spread of the highly contagious disease. And in Canada, data from six jurisdictions shows that the share of 2-year-olds who had received at least one MMR dose fell from nearly 90% in 2019 to less than 83% in 2023.
In South Carolina, there have been at least 22 cases associated with an outbreak in the upstate region, and more than 100 unvaccinated children were quarantined for weeks after a measles exposure at school. The state health department sent a mobile health unit to the area to offer free MMR vaccination, but uptake has been less than leaders had hoped: Only 21 people have utilized the resource over the past week.
“Although we are pleased that 21 people have chosen to receive the vaccine, the noted increase is largely attributed to adults, which contributes less to herd immunity in school populations where we have seen the greatest spread so far during this outbreak,” Louis Eubank, director of the state health department’s Bureau of Emergency Preparedness and Response, said in an email. “We remain hopeful that more parents of unvaccinated children will make an informed decision to take advantage of this opportunity to protect their children from a serious illness.”
The measles outbreak along the state line between Arizona and Utah has grown to more than 100 cases since mid-August, spreading largely in unvaccinated communities. Last school year, nearly 1 in 5 kindergartners in the Southwest district of Utah where the outbreak is growing were missing documentation of having received the MMR vaccine — more than any other region and twice as high as the state average.
As measles has spread across the country and locally, public health officials in Utah report a rise in vaccinations: 32% more MMR vaccinations statewide between March and September than in the same period last year. But vaccinations increased only half as much in the Southwest district — up 16% year-over-year — contributing to widening disparities in coverage.
Researchers from McMaster University say that vaccine hesitancy is fueled by a “complex blend of personal, social and environmental factors.”
Individual behaviors are influenced by community, both in physical proximity and through social media, they said.
“Such dynamics can also result in localized pockets of under-vaccination that benefit the unprotected through herd immunity, but also risk unvaccinated groups becoming high-risk clusters if that protection deteriorates,” they wrote in a recent analysis published in The Conversation. ”The COVID-19 pandemic has proven how damaging misinformation, disinformation, information voids and information gaps can be to public health, including immunization coverage and vaccine hesitancy.”
First Appeared on
Source link