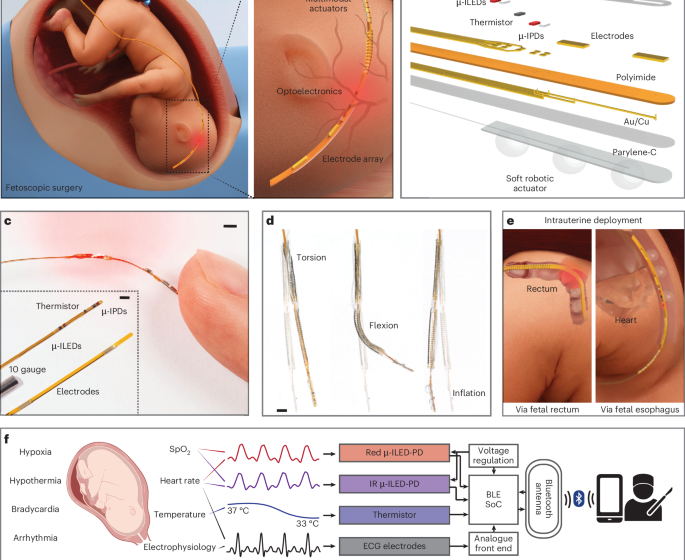
A filamentary soft robotic probe for multimodal in utero monitoring of fetal health
CDC. Birth defects (2024); https://www.cdc.gov/birth-defects/data-research/facts-stats/index.html
Parker, S. E. et al. Updated national birth prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Res. A Clin. Mol. Teratol. 88, 1008–1016 (2010).
Mai, C. T. et al. National population-based estimates for major birth defects, 2010–2014. Birth Defects Res. 111, 1420–1435 (2019).
Wilson, R. D. In utero therapy for fetal thoracic abnormalities. Prenat. Diagn. 28, 619–625 (2008).
Warner, L. L., Arendt, K. W., Ruano, R., Qureshi, M. Y. & Segura, L. G. A call for innovation in fetal monitoring during fetal surgery. J. Matern.-Fetal Neonatal Med. 35, 1817–1823 (2022).
Pinas, A. & Chandraharan, E. Continuous cardiotocography during labour: analysis, classification and management. Best Pract. Res. Clin. Obstet. Gynaecol. 30, 33–47 (2016).
Alfirevic, Z., Devane, D. & Gyte, G. M. Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.cd006066.pub2 (2013).
Neilson, J. P. Fetal electrocardiogram (ECG) for fetal monitoring during labour. Cochrane Database Syst. Rev. 2015, CD000116 (2015).
Symonds, E. M., Sahota, D. & Chang, A. Fetal Electrocardiography. Cardiopulmonary Medicine from Imperial College Press (Imperial College Press, 2001).
Behar, J. A. et al. Noninvasive fetal electrocardiography for the detection of fetal arrhythmias. Prenat. Diagn. 39, 178–187 (2019).
Kahankova, R. et al. A review of recent advances and future developments in fetal phonocardiography. IEEE Rev. Biomed. Eng. 16, 653–671 (2023).
Adithya, P. C., Sankar, R., Moreno, W. A. & Hart, S. Trends in fetal monitoring through phonocardiography: challenges and future directions. Biomed. Signal Process. Control 33, 289–305 (2017).
Wacker-Gussmann, A., Strasburger, J. F. & Wakai, R. T. Contribution of fetal magnetocardiography to diagnosis, risk assessment, and treatment of fetal arrhythmia. J. Am. Heart Assoc. 11, e025224 (2021).
Strasburger, J. F., Cheulkar, B. & Wakai, R. T. Magnetocardiography for fetal arrhythmias. Heart Rhythm 5, 1073–1076 (2008).
Reuss, J. L. Factors influencing fetal pulse oximetry performance. J. Clin. Monit. Comput. 18, 13–24 (2004).
East, C. E., Begg, L., Colditz, P. B. & Lau, R. Fetal pulse oximetry for fetal assessment in labour. Cochrane Database Syst. Rev. 2014, CD004075 (2014).
Donofrio, M. T. et al. Diagnosis and treatment of fetal cardiac disease. Circulation 129, 2183–2242 (2014).
Strasburger, J. F. & Wakai, R. T. Fetal cardiac arrhythmia detection and in utero therapy. Nat. Rev. Cardiol. 7, 277–290 (2010).
Engwall-Gill, A. J. & Perrone, E. E. in Pediatric Surgery (eds Coppola, C. P. et al.) 263–272 (Springer, 2022).
Kohl, T. Minimally invasive fetoscopic interventions: an overview in 2010. Surg. Endosc. 24, 2056–2067 (2010).
Ouyang, W. et al. A wireless and battery-less implant for multimodal closed-loop neuromodulation in small animals. Nat. Biomed. Eng. 7, 1252–1269 (2023).
McCall, J. G. et al. Fabrication and application of flexible, multimodal light-emitting devices for wireless optogenetics. Nat. Protoc. 8, 2413–2428 (2013).
Gutruf, P. et al. Fully implantable optoelectronic systems for battery-free, multimodal operation in neuroscience research. Nat. Electron. 1, 652–660 (2018).
Cianchetti, M., Laschi, C., Menciassi, A. & Dario, P. Biomedical applications of soft robotics. Nat. Rev. Mater. 3, 143–153 (2018).
Konishi, S., Kobayashi, T., Maeda, H., Asajima, S. & Makikawa, M. Cuff actuator for adaptive holding condition around nerves. Sens. Actuators B 83, 60–66 (2002).
Runciman, M., Darzi, A. & Mylonas, G. P. Soft robotics in minimally invasive surgery. Soft Robot. 6, 423–443 (2019).
Kim, Y., Parada, G. A., Liu, S. & Zhao, X. Ferromagnetic soft continuum robots. Sci. Robot. 4, 33 (2019).
Marechal, L. et al. Toward a common framework and database of materials for soft robotics. Soft Robot. 8, 284–297 (2021).
Zhang, Y., Liao, J., Chen, M., Li, X. & Jin, G. A multi-module soft robotic arm with soft actuator for minimally invasive surgery. Int. J. Med. Robot. Comput. Assist. Surg. 19, e2467 (2023).
Coutrot, M. et al. Perfusion index: physical principles, physiological meanings and clinical implications in anaesthesia and critical care. Anaesth. Crit. Care Pain Med. 40, 100964 (2021).
Elgendi, M. Optimal signal quality index for photoplethysmogram signals. Bioengineering 3, 21 (2016).
McCauley, M. D. & Wehrens, X. H. T. Ambulatory ECG recording in mice. J. Vis. Exp. https://doi.org/10.3791/1739 (2010).
Fenske, S. et al. Comprehensive multilevel in vivo and in vitro analysis of heart rate fluctuations in mice by ECG telemetry and electrophysiology. Nat. Protoc. 11, 61–86 (2016).
Hennis, K. et al. In vivo and ex vivo electrophysiological study of the mouse heart to characterize the cardiac conduction system, including atrial and ventricular vulnerability. Nat. Protoc. 17, 1189–1222 (2022).
Chehbani, A., Sahuguede, S., Julien-Vergonjanne, A. & Bernard, O. Quality indexes of the ECG signal transmitted using optical wireless link. Sensors 23, 4522 (2023).
Rahman, S., Karmakar, C., Natgunanathan, I., Yearwood, J. & Palaniswami, M. Robustness of electrocardiogram signal quality indices. J. R. Soc. Interface 19, 20220012 (2022).
Wang, Y., Qu, Z., Wang, W. & Yu, D. PVA/CMC/PEDOT:PSS mixture hydrogels with high response and low impedance electronic signals for ECG monitoring. Colloids Surf. B 208, 112088 (2021).
Versek, C., Frasca, T., Zhou, J., Chowdhury, K. & Sridhar, S. Electric field encephalography for brain activity monitoring. J. Neural Eng. 15, 046027 (2018).
Rosell, J., Colominas, J., Riu, P., Pallas-Areny, R. & Webster, J. G. Skin impedance from 1 Hz to 1 MHz. IEEE Trans. Biomed. Eng. 35, 649–651 (1988).
Goyal, K., Borkholder, D. A. & Day, S. W. Dependence of skin-electrode contact impedance on material and skin hydration. Sensors 22, 8510 (2022).
Lee, S. Y. et al. Evolution and variations of the ovine model of spina bifida. Fetal Diagn. Ther. 50, 491–500 (2023).
Rosén, K. G., Hökegård, K. H. & Kjellmer, I. A study of the relationship between the electrocardiogram and hemodynamics in the fetal lamb during asphyxia. Acta Physiol. Scand. 98, 275–284 (1976).
Westgate, J. A. et al. Do fetal electrocardiogram PR-RR changes reflect progressive asphyxia after repeated umbilical cord occlusion in fetal sheep? Pediatr. Res. 44, 297–303 (1998).
Marwan, A. & Crombleholme, T. M. The EXIT procedure: principles, pitfalls, and progress. Semin. Pediatr. Surg. 15, 107–115 (2006).
Spiers, A., Legendre, G., Biquard, F., Descamps, P. & Corroenne, R. Ex utero intrapartum technique (EXIT): indications, procedure methods and materno-fetal complications—a literature review. J. Gynecol. Obstet. Hum. Reprod. 51, 102252 (2022).
Chen, G., Zhu, Z., Liu, J. & Wei, W. Esophageal pulse oximetry is more accurate and detects hypoxemia earlier than conventional pulse oximetry during general anesthesia. Front. Med. 6, 406–410 (2012).
Phillips, J. P., Kyriacou, P. A., Jones, D. P., Shelley, K. H. & Langford, R. M. Pulse oximetry and photoplethysmographic waveform analysis of the esophagus and bowel. Curr. Opin. Anesthesiol. 21, 779 (2008).
Varcoe, T. J. et al. Fetal cardiovascular response to acute hypoxia during maternal anesthesia. Physiol. Rep. 8, e14365 (2020).
Fong, D. D. et al. Validation of a novel transabdominal fetal oximeter in a hypoxic fetal lamb model. Reprod. Sci. 27, 1960–1966 (2020).
Park, J., Seok, H. S., Kim, S.-S. & Shin, H. Photoplethysmogram analysis and applications: an integrative review. Front. Physiol. 12, 808451 (2022).
Elgendi, M. On the analysis of fingertip photoplethysmogram signals. Curr. Cardiol. Rev. 8, 14–25 (2012).
Abushouk, A. et al. The dicrotic notch: mechanisms, characteristics, and clinical correlations. Curr. Cardiol. Rep. 25, 807–816 (2023).
Inoue, N. et al. Second derivative of the finger photoplethysmogram and cardiovascular mortality in middle-aged and elderly Japanese women. Hypertens. Res. 40, 207–211 (2017).
Hashimoto, J. et al. Pulse wave velocity and the second derivative of the finger photoplethysmogram in treated hypertensive patients: their relationship and associating factors. J. Hypertens. 20, 2415–2422 (2022).
Street, P., Dawes, G. S., Moulden, M. & Redman, C. W. G. Short-term variation in abnormal antenatal fetal heart rate records. Am. J. Obstet. Gynecol. 165, 515–523 (1991).
Young, B. K., Katz, M. & Wilson, S. J. Sinusoidal fetal heart rate. I. Clinical significance. Am. J. Obstet. Gynecol. 136, 587–593 (1980).
Partridge, E. A. et al. An extra-uterine system to physiologically support the extreme premature lamb. Nat. Commun. 8, 15112 (2017).
Kabagambe, S. K. et al. Lessons from the barn to the operating suite: a comprehensive review of animal models for fetal surgery. Annu. Rev. Anim. Biosci. 6, 1–21 (2017).
Petersen, R., Connelly, A., Martin, S. L. & Kupper, L. L. Preventive counseling during prenatal care: Pregnancy Risk Assessment Monitoring System (PRAMS). Obstet. Gynecol. Surv. 56, 599–601 (2001).
Veena, S. & Aravindhar, D. J. Remote monitoring system for the detection of prenatal risk in a pregnant woman. Wirel. Pers. Commun. 119, 1051–1064 (2021).
Haga, Y. et al. Small diameter hydraulic active bending catheter using laser processed super elastic alloy and silicone rubber tube. In 2005 3rd IEEE/EMBS Special Topic Conference on Microtechnology in Medicine and Biology 245–248 (2005).
Liao, Z. et al. On the stress recovery behaviour of Ecoflex silicone rubbers. Int. J. Mech. Sci. 206, 106624 (2021).
Fung, Y.-C. in Biomechanics: Mechanical Properties of Living Tissues 321–391 (Springer, 1993).
Fang, Q. & Boas, D. A. Monte Carlo simulation of photon migration in 3D turbid media accelerated by graphics processing units. Opt. Express 17, 20178–20190 (2009).
Yu, L., Nina-Paravecino, F., Kaeli, D. & Fang, Q. Scalable and massively parallel Monte Carlo photon transport simulations for heterogeneous computing platforms. J. Biomed. Opt. 23, 010504–010504 (2018).
Lu, W. et al. Wireless, implantable catheter-type oximeter designed for cardiac oxygen saturation. Sci. Adv. 7, eabe0579 (2021).
Bosschaart, N., Edelman, G. J., Aalders, M. C. G., Leeuwen, T. G. V. & Faber, D. J. A literature review and novel theoretical approach on the optical properties of whole blood. Lasers Med. Sci. 29, 453–479 (2014).
Khan, R., Gul, B., Khan, S., Nisar, H. & Ahmad, I. Refractive index of biological tissues: review, measurement techniques, and applications. Photodiagnosis Photodyn. Ther. 33, 102192 (2021).
Morrison, J. L. et al. Improving pregnancy outcomes in humans through studies in sheep. Am. J. Physiol. Regul. Integr. Comp. Physiol. 315, R1123–R1153 (2018).
Joyeux, L. et al. Validation of the fetal lamb model of spina bifida. Sci. Rep. 9, 9327 (2019).
Zhou, J. et al. Data and code for the article ‘A filamentary soft robotic probe for multimodal in utero monitoring of fetal health’. Zenodo https://doi.org/10.5281/zenodo.17371614 (2025).
First Appeared on
Source link






