
Medications taken by HALF of Americans raise risk of cancer years after you stop taking them
Some of the most common medications taken by tens of millions of Americans leave a lasting impact on the body long after a person stops taking them, according to new research.
Beta-blockers, commonly prescribed for high blood pressure and heart conditions, were linked to changes in gut bacteria that were detectable even when people had stopped taking them several years earlier, according to a new study by Estonian researchers.
The same held true for anti-anxiety medications, part of the benzodiazepine class, including Xanax and Valium. Antidepressants had similar carryover effects, as did proton pump inhibitors, medications millions take for acid reflux and heartburn.
The microbiome is the body’s collection of beneficial bacteria. Its health relies on a diverse population of bacteria to fight disease, absorb nutrients and regulate immune and metabolic systems. It is influenced by everything from diet and lifestyle to the medications a person takes, including common prescription drugs.
The new study confirmed that commonly prescribed medications, ranging from antibiotics to antidepressants, consistently reduce the diversity of gut bacteria, sometimes for years.
A less diverse microbiome is linked to a weaker gut barrier, chronic inflammation and a compromised immune system. This state of imbalance, known as dysbiosis, creates a state of chronic inflammation and weakened immune defense that is a recognized breeding ground for cancer development, specifically, colorectal cancer.
Dysbiosis creates a gut environment dominated by cancer-promoting bacteria, which can trigger tumor growth by stimulating blood vessel formation, uncontrolled cell division and the evasion of cell death.
The Estonian team’s findings impact tens of millions of Americans. Annually, hundreds of millions of antibiotic prescriptions are written, while about 30 million people each take benzodiazepines, beta-blockers or SSRIs (stock)
To investigate the long-term effects of medications on gut bacteria, an Estonian study genetically analyzed stool samples from 2,509 adults.
By revisiting 328 of them four years later with new samples and checking their prescription records, they pinpointed the effects of common drugs like acid reflux pills, antidepressants and anxiety medications.
Ninety percent of 186 medications tested disrupted the gut microbiome, and for many, including antibiotics, antidepressants and proton pump inhibitors, the effects persisted for over three years after the last dose.
Antibiotics have the most severe and long-lasting impact on the gut microbiome. The study found that the effects of drugs like azithromycin and penicillin remain detectable for over three years.
The reduction in bacterial diversity from antibiotics never fully recovered, suggesting the damage is permanent or lasts for many years.
Like antibiotics, benzodiazepines were associated with fewer species of bacteria, changing the overall composition of the gut microbiome.
The drugs’ effects persisted for over three years and were cumulative, with more prescriptions leading to greater gut imbalance.
Among all non-antibiotic drugs, beta-blockers were one of the top disruptors of the gut microbiome, accounting for a significant portion of the variation in people’s gut bacteria.
Proton-pump inhibitors (PPIs) also caused long-term damage to the gut microbiome, reducing diversity and creating a pro-inflammatory state that can fuel cancer.
These changes to people’s microbial ecosystems persisted for years after people stopped taking the medication.
The second round of testing, though smaller, solidly proved that proton pump inhibitors and various antibiotics also have lasting impacts on the gut microbiome.
A dysbiotic gut often has a ‘leaky’ barrier, allowing bacteria and their toxins to enter the bloodstream. This triggers a persistent, low-grade inflammatory state throughout the body.
A depleted microbiome is less effective at detoxifying harmful compounds and produces lower levels of protective molecules like butyrate, leaving the body more vulnerable to exposures or events that damage the cells’ DNA and can initiate the development of cancer.
Researchers deduced in 2024 that changes in the gut microbiome, including the proliferation of bad bacteria, including some previously unknown strains, has been linked to between 23 and 40 percent of colorectal cancer cases.
They proved that these newly discovered bacteria can directly trigger the growth of precancerous growths in the colon.
They also found that the gut microbiome can create a pre-cancerous environment by causing changes in colon cells that are crucial for the structural integrity of tissues.
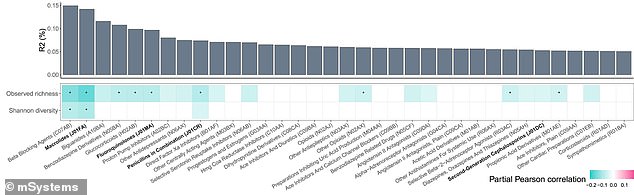
The bar graph portion of the graphic shows that beta-blockers were the top disruptor. The study used a color-coded chart (in shades of blue below) to show that most common medications are strongly linked to a major loss of gut bacterial diversity. Darker shades of blue indicated a stronger negative correlation
Dr. Oliver Aasmets of the University of Tartu Institute of Genomics and lead author of the latest Estonian study, said in a statement: ‘Most microbiome studies only consider current medications, but our results show that past drug use can be just as important as it is a surprisingly strong factor in explaining individual microbiome differences.’
Their findings were published in the journal mSystems.
These findings apply to tens of millions of Americans. In the US, healthcare providers wrote approximately 270 million antibiotic prescriptions.
Around 30 million Americans take benzodiazepines and 30 million take beta-blockers. Further, approximately 30 million Americans take SSRIs.
First Appeared on
Source link






